
Wearable Devices for Lifestyle and Medical Monitoring: Technical and Research Challenges
This article is the third article in our article series titled “Wearable Devices for Lifestyle and Medical Monitoring”. …

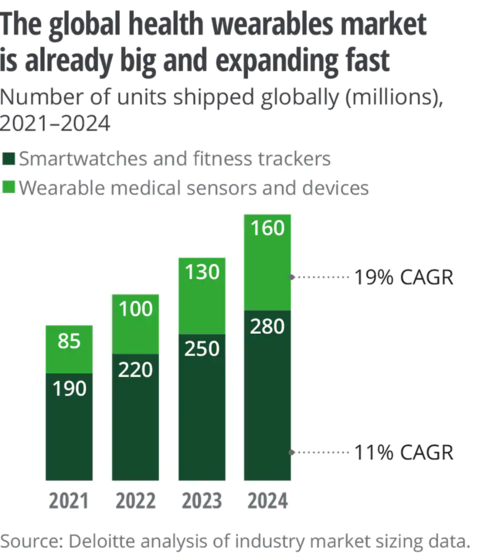
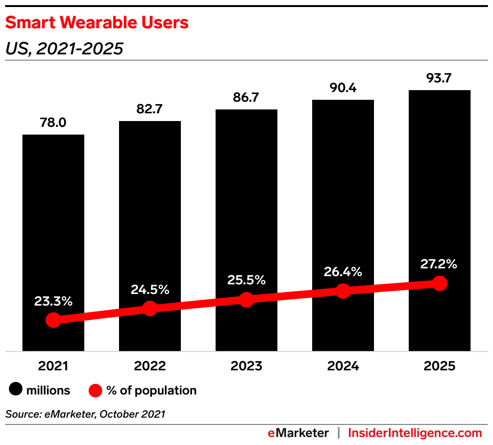
Wearable technology has begun to see an explosion in adaptability over the last decade, both in public and in healthcare settings. Coupled with the rise in innovation that supports more comfortable hardware, tools to gather nuanced findings without compromising performance, new software capabilities, ease of use, and the interoperability of each new product, a vital new data source for providers and patients to learn about individual health has emerged. Deloitte Insight analysis has predicted that about 320 million consumer health and wellness devices with wearable functionality will be present within the market – in line with the current demand, with upwards of 440 million offerings being seen in the next three years [1]. eMarketer estimates that more than a quarter (27.2%) of the United States population will possess at least one wearable by 2025 [2]. The continual trends of innovation have created versatile tools which collect the same data as medical-grade devices, increasing the brevity and resolution of vital metrics that can provide information about everyday life, often at comparably similar resolutions to those obtained in a clinical setting.
The scope of data collected by the most worn devices can be simple yet immensely capable of providing utility for providers. Users’ most utilized metrics are activity levels – particularly steps counted, next to heart health and workout capacity (with heart rate being most cited), sleep quality/duration, and calories consumed [3]. These metrics may appear simple, but these nuanced data demonstrate the impact of a healthy sleep cycle, diet, and exercise regimen on multiple facets of individual physical and mental well-being – broadening the potential that tracking and understanding these metrics can have on personal health [4,5,6].
Complimentary software innovations have diversified the breadth of these metrics by providing more analytics by extending the capabilities of existing hardware. A recent primary example is sleep-phase tracking released with apple watch OS 9 (September of 2022), which takes advantage of already installed sensors on watch series six and beyond to essentially establish a portable polysomnography device by implementing machine learning algorithms that predict sleep phase – complimented by heart rate and respiratory rate recorded at regular intervals from sensors already installed [7]. It thereby is not a stretch to consider that such technology may eventually allow for sleep apnea tracking to be attempted at home through these devices with remarkable accuracy in the coming years, opening an avenue to intervene in these patients more effectively.
In the clinical setting, assessments on many of the broadest metrics of individual health: activity, sleep, and diet begin with binary questions. Either a yes or no to determine if there are any issues, and if yes, then probing can be done. Yet this entire paradigm relies on the provider’s ability to understand the patient’s nuances and ask the right subjective questions while the patient’s recollection of their symptoms, which often becomes a summarization, serves as their guide. Each influence becomes highly subjective, and thereby, assessment of patient health becomes relative rather than a standardized approach, which otherwise would allow for objective evaluation and iterated improvement. Furthermore, there is a broad consensus that sleep, activity, and diet affect a broad spectrum of one’s health, whether in a disease state or for preventative purposes, yet they can become challenging to initiate a discussion on. One primary barrier to beginning any conversation on these vital metrics can be the work required to ascertain enough data to make any meaningful conclusion. The time spent during each visit, such as in an outpatient primary care setting, is also shared with other parts of the health evaluation, such as doing an essential comprehensive physical examination.
Optimizing individual health through bettering activity, sleep, and diet metrics can have innumerable positive effects on personal health, but these vital discussions have yet to be done without impeding the limited time each provider has with their patient. These issues are where wearables can begin to kickstart an evolution in the potential for providers to understand their patients. Wearable devices have already started to demonstrate a capability in providing accurate real-time continuous metrics that have been utilized by individuals to better their health over a variety of populations [8,9]. The implications of wearables for clinical practice begin to emerge by taking advantage of the device’s ability to provide real-time insight into the patient status rather than episodic anecdotal inference dependent upon the patient’s recollection – allowing for true objectivity to be introduced when making an assessment and treatment plan.
The most effective patient-physician relationships are based on effective communication, but the constraints of discussing the topics of sleep, activity, and diet due to their complexity may only leave a superficial understanding by the provider at the end of the visit. While wearable data can provide a source of complex, enriching understanding, the problem for providers to spend time delving into them during a patient visit can also emerge. Providers may often have to navigate to their health apps, and physicians must then spend time siphoning through charts to understand the trends within these applications – which users outside of the clinic have time for but become limited during patient acute patient visits. If patients use multiple devices, each with its own applications, the problem is compounded.
The ubiquity of wearables has constructed new avenues for clinicians, yet their introduction into the clinical setting already faces barriers surrounding the theme of how to fit them into what is already a congested visit. Observational and cohort studies among primary care physicians have shown that the average time providers spend for actual communication and visit times ranging from 6.3-17.2 minutes, and within visits addressing multiple problems, with on average, 1.1 minutes spent behind each complaint [10,11]. Each problem then involves acquiring a thorough history based on the patient’s personal accounts, necessitating a provider to be skilled in understanding the right nuances to probe for while also depending on the patient’s recollection.
Such visit times can only be effective when a designated problem is discussed by the provider to ensure visits have a primary focus on the patient’s current problem, often forgoing details of any other chronic co-morbidities which can conflict with patients who have a more significant burden of disease/multi-disease that require regular care. While this model of care strikes a balance between provider availability and addressing patients’ complaints in practice, the interim time between visits can contribute to a worsening of status, increase the likelihood of new complications, and worsen the burden of resources on the patient and, if applicable, their caregiver.
The interim time between each visit is also a lived experience for patients, who experience their own health fluctuations from their baseline, which could be vital to providers. Attempting to collect these points only services add further burden on providers and prevent a focused and effective visit from actualizing. Data obtained from wearables can thereby assist in providing deeper resolution by filling in these gaps and increasing collection frequency which is otherwise difficult to address. Even during routine annual wellness visits, queries regarding sleep and activity levels depend on how to open a patient is in discussing these issues, often not probed further if nothing of concern is shared. Thereby the implications of wearables for clinical practice begin to emerge from their ability to provide the continuous stream, even during interim visits, without being dependent upon the patient’s recollection. All that is required is the ability to implement these findings into clinical practice without increasing the burden placed on the providers.
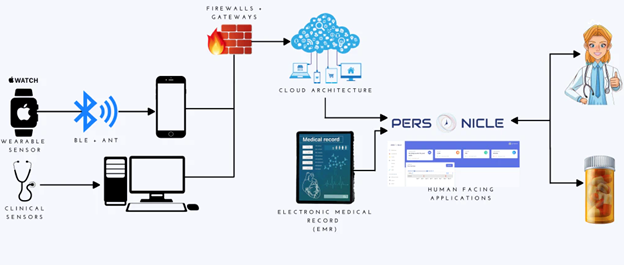
Providing a mechanism to organize and present wearable data in an easily ingested format can produce an avenue for practical adaptability by healthcare professionals. The innovations made with the Personicle charts are a means to integrate wearable data as a source for patient evaluation into clinical practice without friction.
Almost all the most popular wearable devices, including the Fitbit, Apple Watch, Samsung products, and the Oura ring, have relatively the same kinds of data collected whilst having similar hardware capabilities. This means that devices that most patients would use regardless of if they are different between each patient, and that data that they collected between them, is relatively homogenous, but the problem of working through each one during a patient visit can become easily daunting for healthcare practitioners. Providing a central hub to intuitively present this data from any potential device establishes a unified source, eliminating the friction from referring to multiple device-specific applications and opening an avenue to integrate wearable data as a part of the assessment and plan. The structure of Personicle allows it to be a use case for this exact purpose.
A Personicle, or a personal chronicle, is a collection of all lifestyle data obtained from any wearable device or publicly available data source of an individual into one platform, which is presented in an intuitive and digestible form factor that continues to evolve for both personal and professional use.
Within the healthcare setting and for providers’ usage, data collected by any supported wearable will be presented in each patient’s Personicle. The metrics are not only limited to specific types but can include all data, including basic analytics that are done by the device to provide more excellent resolution to each metric. Furthermore, data not presented explicitly on these wearables but can still illuminate other aspects of patient health – including the social determinants of health are included as sources, cross-referenced with publicly available climate and government databases recording obtainable components of a patient’s social determinants of health.
As the capabilities of wearables continue to increase in their ability to capture data with better accuracy, establish new sources of data, and add novel software additions which tap into the potential for nuanced analytics, Personicle will continue to evolve in pace. Utilizing Personicle as a means of understanding patient health metrics from wearables will simultaneously keep providers updated without any extra effort on their part, essentially automating the effort required to keep up to date with this process by leveraging the ability for the software to update in lockstep with industry innovation.
For providers to be effective, they need to ask the right questions to patients to get a sense of how they are feeling. Objective data does have its utility, which is why hospital admissions, for example, can rely on lab values, routine vital checks, and imaging for conclusive results, but supplementing those findings with conversation can provide a context to them and inform decision-making. This role makes healthcare providers serve as their data collectors and analysts. From medical school training, there is an emphasis placed on understanding pathologies, not just for the sake of recognizing them on examinations or evaluations but also as a means of guiding differential thinking by helping to reason out the best queries to ask patients.
While this model is exceptionally vital to successfully treating and diagnosing conditions, it can be challenging to do the same effect for a healthy patient or a patient with chronic pathologies. In these evaluations, especially when providers have not had a long history with the patient, queries to understand their patients’ health and experiences are limited in their effectiveness. “Do you sleep on average of 8 hours per day?” for example, can be a helpful question, but patients might consider 8 hours from the time they lay in bed (for which they are initially awake) rather than when they feel asleep (which is impossible to tell) and wake up. Furthermore, responses can be complicated by a lack of recollection, where the accuracy of each incident often cannot be recalled, and thereby a summarized response is then given. This can prevent any nuances of concern from rising and being addressed. This means that the more profound the delve into the problem (the deeper the data collection), the harder it can be to get the “type” of data needed to make the best analysis by the provider, yet it is within these depths that the true scope of any health problem can be understood in the context of each patient – since everyone has different experiences.
These factors necessitate that for a more personalized healthcare system to emerge, the individual providers that make that system must be empowered with the tools to assist in gathering personalized health status data without increasing the burden of work. In an already congested healthcare visit with an efficient practice, providers can be disincentivized in heeding attention to every single problem on a personal level if adds immense friction to the workflow. As is, a balance is often struck between addressing patient concerns and seeing the day’s list in proper time, which disincentivizes extended visits. The advent of wearables and their ubiquity in adaptability has now provided a road to circumvent these concerns. This objective means of assessing a patient’s health can lower the effort required to address lifestyle data in a routine clinical evaluation by not necessitating these queries to be asked of the patient.
Most of the questions providers may ask to understand a patient’s status may already be usefully recorded, accurately, in real-time without any reliance on patient recollection by wearables. Here, one key role Personicle can serve is to function as a digital data collecting assistant for providers, empowering them to understand the nuances of their patients without sacrificing efficiency.
It can be easy to assume that as wearables improve and more diverse data sources emerge, Personicle’s ability to present them may make it tempting for an accurate history to not be taken. Yet, the very nature of history taking relies on the ability of providers to assess the patient’s clinical picture or complaint of concern. Data sources can point to what is wrong, but the creative processes required to determine the priority of problems to solve and establish connections that may facilitate treatment on multiple fronts from minimal changes cannot be eclipsed by simply recording as much data as possible. Provider intuition and synthesis of all available data are what drive the most effective and innovative treatment strategies, but Personicle can still serve as a powerful companion to the modern provider.
As a clinical tool, it increases the amount of data available to providers without the extra effort required to collect it. Most importantly, it brings to attention data points that can contribute to multiple facets of a patient’s health in real-time synchronous recordings without compromising accuracy over any required period. Through this paradigm, Personicle can empower providers to easily practice personalized medicine on a continually increasing scale – taking advantage of the unprecedented revolution in wearables that we are seeing today.

This article is the third article in our article series titled “Wearable Devices for Lifestyle and Medical Monitoring”. …

This article is the second in our article series titled “Wearable Devices for Lifestyle and Medical Monitoring”. Readers …